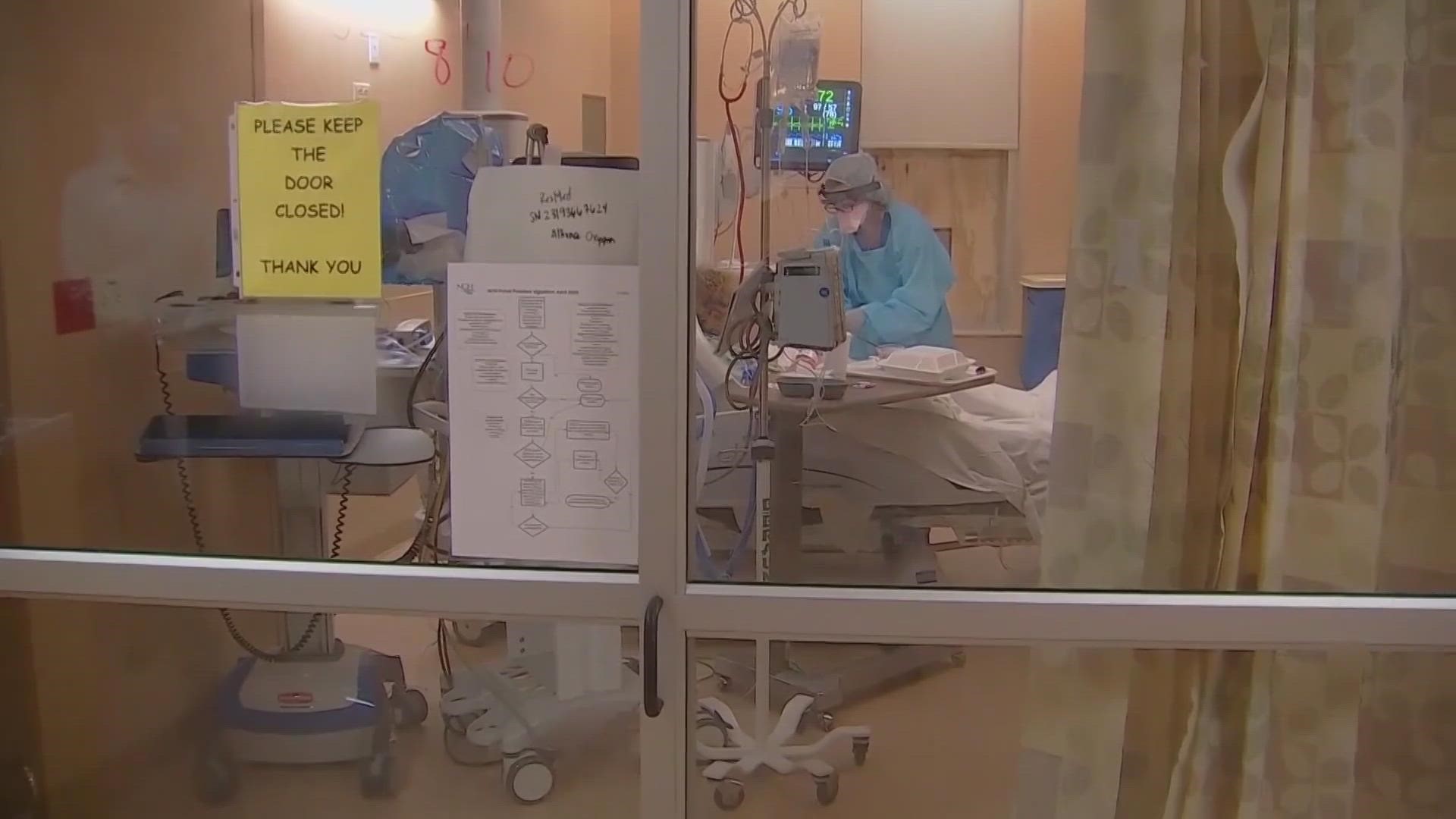
GREENSBORO, N.C. — People who use Medicaid and have a severe mental illness or developmental disability may be at risk of losing their doctors.
They need their providers to agree to be part of the coverage network.
2.3 million people in North Carolina use Medicaid.
State lawmakers tell us about 150,000 people would use Tailored Plans but there have been issues getting doctors to sign on.
These Tailored Plans provide care for people with significant mental health illnesses, developmental and intellectual disabilities, and substance use issues.
Leann Henkel uses Medicaid for her son, Blake who's autistic.
“It’s very difficult and very exasperating. There have been so many parents calling this week. What are you going to do? What are you going to choose not knowing what to do and having very little information,” Henkel explained.
As of right now, there aren't enough healthcare providers in the network with the new plan to provide adequate coverage for people.
If a doctor's office does not sign on with this new plan, patients could be forced to change doctors or may even have to pay out of pocket.
State Representatives Larry Potts and Pricey Harrison urge people to reach out to their local elected officials if they have concerns.
"I talked to the secretary of DHHS about it today, and he assured me before the plan goes live that there will be a network adequacy by county," Representative Potts said.
Representative Harrison added, "federal law requires that managed care plans have an adequate number of providers to serve all of the beneficiaries."
This is still worrisome for many people like Henkel who have trouble finding new in-network providers for their sons.
"Practices where we don't know the doctors, they don't know our children and it's gonna be very hard on them to acclimate to new people, new environment and having to explain the medical histories, and the things that are important for our child health," Henkel said.
The state already delayed the launch of tailored plans once, pushing the date from Dec. 1, 2022, to April 1 because they didn't have enough healthcare providers signed on.