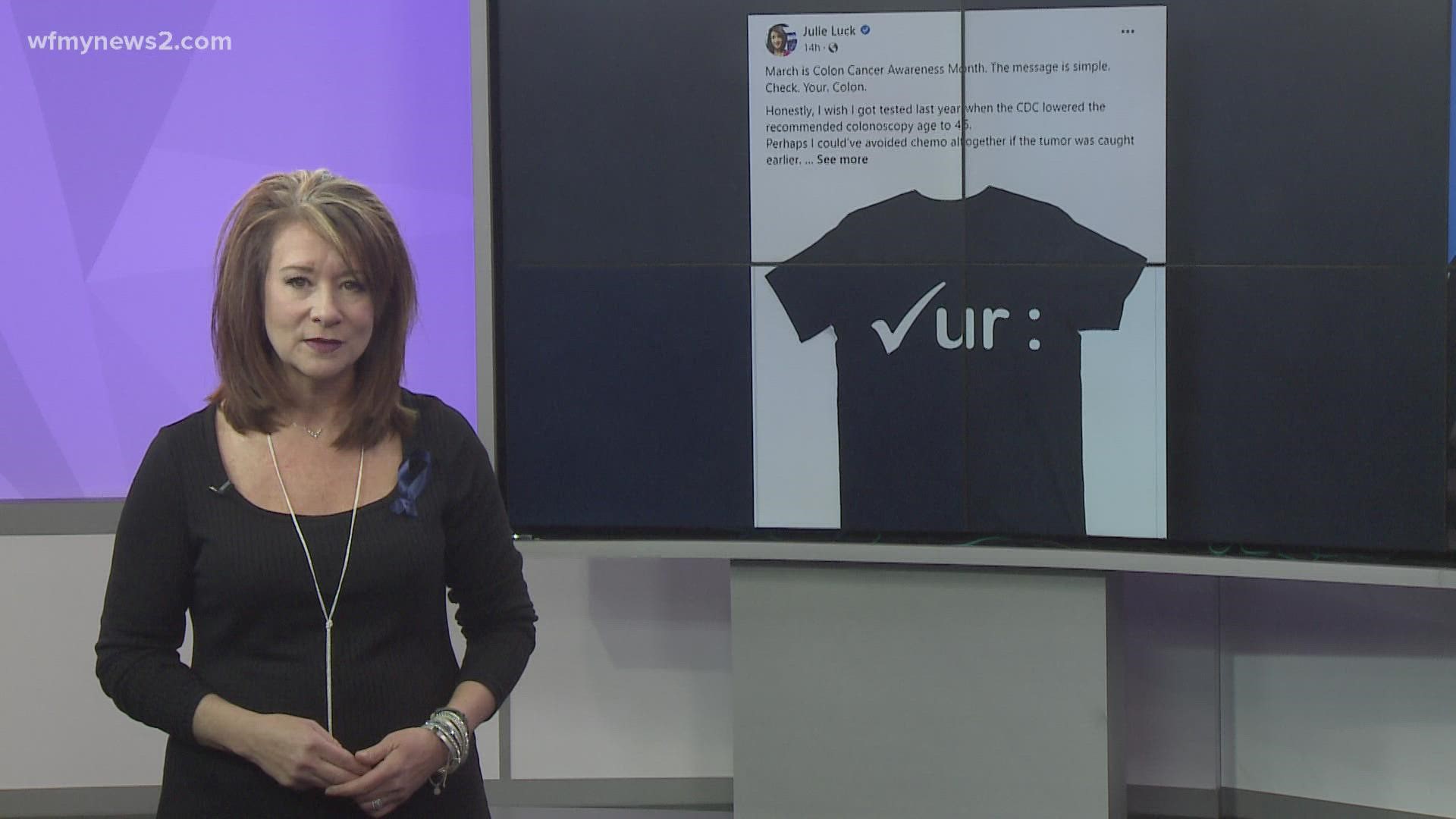
March is Colon Cancer Awareness Month and we're fighting alongside WFMY News 2’s Julie Luck as she battles her own fight with colon cancer while going through chemotherapy.
More than 50,000 Americans die each year from colorectal cancer, and the number is growing rapidly for those under the age of 50, according to the Colorectal Cancer Alliance.
That's why it's so important to get screened. Here are six questions and answers to know when it comes to screening from the Colorectal Cancer Alliance.
1. How does screening save lives?
A: Screening for colorectal cancer works in two ways:
- By finding cancers early when treatment is most effective
- By finding growths (polyps) inside the colon and removing them before they become cancer
2. If screening works then why aren’t more people doing it?
A: According to the Centers for Disease Control and Prevention, only 1 in 3 adults who need to be screened are actually doing it. Why so few? There are many reasons, including:
- Insurance coverage and paying for the test
- Fears about the test or preparation
- A primary care doctor hasn’t suggested it. (Please be your own advocate! Know your options!)
- Too busy/don’t think they have time
3. What should you do if you can’t afford to pay for a screening test or the costs associated with it?
A: It’s important to be aware that under the Affordable Care Act, screening colonoscopies are covered as a preventative measure for average risk populations with insurance. We recommend talking to your doctor, insurance provider or local gastroenterologist to learn more about your coverage and financial assistance options they may have.
The Screening Resources page also includes references to help you find federally-funded or low-cost screening resources if you are uninsured.
If you're unable to pay for a screening test, check out our Blue Hope Financial Assistance Program.
4. Why remove polyps if you don’t have colon cancer?
A: Polyps are growths that may turn into colorectal cancer over time. While not every polyp turns to cancer, it is difficult to know which ones will. Also, almost every colorectal cancer begins as a small non-cancerous polyp. The good news is that during colonoscopy, these polyps can be identified and removed, preventing a possible colorectal cancer diagnosis. If a polyp is large enough, tissue can be taken and sent for biopsy to determine the exact type of polyp.
5. Why does the type of polyp matter?
A: Not all polyps are created equal. There are four types of polyps that commonly occur within the colon and rectum:
- Inflammatory - Inflammatory polyps are most often found in patients with ulcerative colitis or Crohn's disease. Often called "pseudopolyps" (false polyps), they are not true polyps, but just a reaction to chronic inflammation of the colon wall. They are not the type that turns to cancer. They are usually biopsied to verify type.
- Hyperplastic - Hyperplastic polyps are common, usually very small and often found in the rectum. They are considered to be low risk for cancer.
- Tubular adenoma or adenomatous polyps - These are the most common type of polyp and are the ones referred to most often when a doctor speaks of colon or rectal polyps; about 70% of polyps removed are of this type. Adenomas carry a definite cancer risk that rises as the polyp grows larger. Patients with a history of adenomatous polyps must be periodically reexamined.
- Villous adenoma or tubulovillous adenomas - Villous and tubulovillous adenomas polyps account for about 15% of the polyps that are removed. These are the most serious type of polyps with a very high cancer risk as they grow larger.
6. Who should I call if I have questions about colon cancer screening?
A: If you have questions about specific screening tests, who should be screened and when, or anything else related to colon cancer screening, we encourage you talk with your doctor or call our toll-free Helpline at (877) 422-2030.